Why We Need Arabic Language Models
24 August 2025
Published online 11 September 2024
Study reveals response to deadly 2022 outbreak was complicated by difference in virulence and resistance, demanding varied protocols
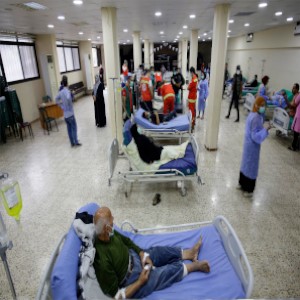
Lebanon’s cholera outbreak of 2022, the country’s first in 30 years, was caused by two different strains of bacteria, resulting in 8,007 suspected cases, 671 confirmed cases, and 23 deaths, a study published in Nature Communications revealed.
Cholera is an acute infectious disease in the digestive system that causes severe diarrhea and dehydration, and potential death if not treated quickly. Lebanon had faced several outbreaks of cholera throughout history, but this the first to be caused by two strains.
Ghassan Matar, professor in the Department of Experimental Pathology, Immunology and Microbiology at the American University of Beirut, and co-author of the study, says outbreaks are usually caused by a single strain (genotype) of Vibrio cholerae.
“Specific conditions that allow multiple strains to coexist and interact complicate the dynamics of the outbreak and disease management. These should be taken into account during epidemiological investigations and response strategies,” Matar says.He stresses that the study findings confirm the need to use genomic surveillance in tracking and monitoring cholera.
Epidemiological study
The team conducted a comprehensive genetic epidemiological study of 34 clinical and environmental samples isolated from the Lebanon outbreak. They found that the dominant strain was linked to a subspecies from South Asia and Africa called AFR15, while the second, less common strain is highly drug-resistant and linked to isolates of a subspecies from Yemen called AFR13.
The two strains showed different patterns of antimicrobial resistance; the main strain had a narrow resistance spectrum, while the second strain showed broad resistance to several antibiotics, including third-generation cephalosporins and macrolides. This difference in virulence and resistance brought complex public health impacts, and worsened the challenge of controlling the outbreak and providing effective treatment.
The strain diversity also demanded advanced detection tools, making it difficult to accurately monitor the outbreak. Treatment protocols had to be modified according to each strain, adding further complexity to the response.
“Antibiotic-resistant cholera strains pose a major threat to public health because of the difficulty of treatment and the increased risk of complications and deaths,” said Taher El-Demerdash, a professor of tropical medicine at Tanta University in Egypt, who was not involved in the study.
Al-Demeerdash recommends implementing preventive measures that include monitoring strains, and educating communities about transmission and the importance of appropriate treatment.
Matar stresses the need to improve laboratory capabilities and develop advanced diagnostic tools, as well as greater investment in water and sanitation infrastructure.
It is equally critical, Matar adds, to expand vaccine coverage in vulnerable areas, developing tailored response plans for multi-strain outbreaks, and enhancing international and regional cooperation to share data and coordinate efforts.
Link to original article is here.
doi:10.1038/nmiddleeast.2024.285
Stay connected: